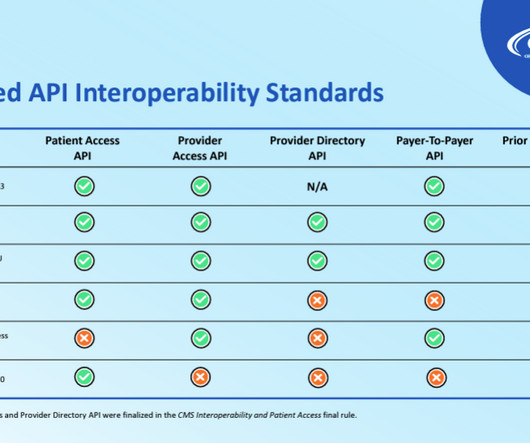
CMS Finalizes its Proposal to Advance Interoperability and Improve Prior Authorization Processes
Healthcare Law Blog
JANUARY 26, 2024
Merit-based Incentive Payment System (“MIPS”) eligible clinicians, operating under the Promoting Interoperability performance category of MIPS, and eligible hospitals and critical access hospitals (“CAHs”), operating under the Medicare Promoting Interoperability Program, are impacted by the Final Rule, as well.









Let's personalize your content