 By Yuriy Pylypchuk and Wes Barker, ONC
By Yuriy Pylypchuk and Wes Barker, ONC
Twitter: @ONC_HealthIT
In 2020, as the U.S. health care system faced the unprecedented challenge of combating the COVID-19 pandemic, telemedicine emerged as an invaluable care delivery tool; both providers and patients heavily relied on it for providing and receiving care. Through an analysis of National Electronic Health Record Survey (NEHRS) 2021 data and from in-house data collected from electronic health record (EHR) developers’ app galleries, we have an opportunity to inform the public about physicians’ experiences with telemedicine during the pandemic.
Physicians’ use of telemedicine increased remarkably in 2021
New data show that the percent of physicians that used telemedicine jumped from 15 percent in 2018 and 2019 to 87 percent in 2021, underlining the unprecedented need for telemedicine during this time. Although the majority of physicians used telemedicine for delivering some care in 2021, most patient visits remained in-person. For example, 53 percent of physicians used telemedicine for less than 25 percent of their patient visits while only nine percent of physicians used telemedicine for 50 percent or more of their patient visits.
Large variation in telemedicine use exists across physician characteristics
There are significant differences across physician characteristics in their use of telemedicine. Small practices (three physicians or fewer) were 20 percent less likely to use telemedicine than large practices (more than 50 physicians). Practices owned by individual physicians or physician groups were less likely to use telemedicine than those owned by insurance companies or medical centers. Primary care physicians were 17 percent more likely to use telemedicine than surgical specialists. These differences mirror the type of telemedicine tools used, especially telemedicine platforms integrated with EHRs.
There was a similar usage of telemedicine among physicians residing in rural and urban areas. Telemedicine has emerged as an invaluable mechanism of delivering care, and the data show that rural physicians use the technology at the same rates as their urban-based peers. As telemedicine provides access to care to rural patients who must long travel distances and may live in an area with provider shortages, the results are heartening.
A number of factors can explain differences across physician characteristics and merit further investigation. For example, a lack of resources may explain lower usage of telemedicine among small practices compared to large ones while high patient demand for this tool and the nature of care delivery may explain higher usage of telemedicine among primary care physicians compared to surgical specialists.
Barriers to telemedicine and the role of quality
Physicians indicated that patients’ challenges with using telemedicine (such as difficulty using and accessing technology) were the most common barriers to their use of telemedicine. Other issues such as limited internet access and difficulties using telemedicine platforms inhibited physicians’ use of telemedicine to a lesser extent.
Figure 1: Percent of physicians satisfied with telemedicine and believe telemedicine provides similar quality of care to an in-person visit by having telemedicine platforms integrated and not integrated with their EHRs, 2021.
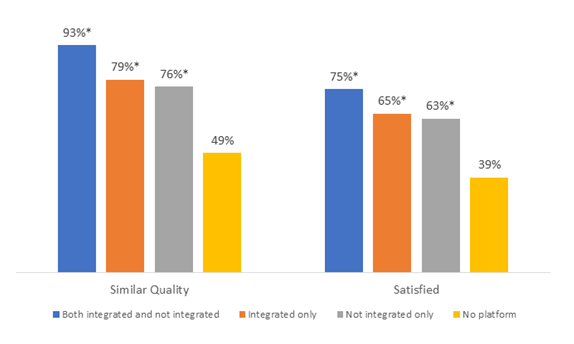
Source: National Electronic Health Record Survey.
Notes: Estimates are calculated on the sample of office-based physicians who use telemedicine. Similar quality is defined as physicians who indicated that use of telemedicine provides similar quality of care to an in-person visit ‘Fully’, ‘To a great extent’, or ‘To some extent’. Satisfied is defined as physicians who indicated they are ‘Very satisfied’ or ‘Somewhat Satisfied’ with the use of telemedicine. ‘No platform’ is defined as physicians who used telemedicine tools other than telemedicine platforms integrated or not integrated with their EHR. *Significantly different from “No Platform” within each category, * p<0.05.
There was a clear relationship between physician satisfaction with telemedicine usage and the type of telemedicine tool used. Physicians who used a telemedicine platform, integrated or not integrated with their EHR, were more likely to be satisfied with the use of telemedicine (75 percent) than physicians who only used phone or video conference tools (39 percent) (Figure 1). Similarly, physicians who used both EHR-integrated and not integrated platforms were more likely to report that telemedicine provides a similar quality of care to in-person visits than physicians who used phone or video conference tools alone. These results may indicate the strength of certain technologies to provide virtual care of similar quality to in-person care.
Rapid growth of telehealth apps
Unsurprisingly, the growth in telemedicine demand was met with an increase in the availability of telemedicine technology at the point of care. An analysis of EHR market leaders’ health app marketplaces showed a rapid rise in the number of telemedicine apps available to EHR users during the pandemic. The number of new apps that integrate with an EHR doubled from January 2020 to June 2021. Half of the new apps provided some form of video conferencing, while the other half did not, providing a mix of text messaging, audio communication, and non-communication capabilities. These data show the broad types of functionalities available through these apps, providing even more details about how these apps virtualized care during this period.
Beyond providing virtual methods of communication between provider and patient, the apps also enabled online scheduling, patient monitoring, and tools for automating provider tasks. The varied functionalities show that telemedicine goes beyond just virtual communication and endeavors to enable more care delivery and care management in the palm of your hand and in the comfort of your home. These results reflect the industry’s robust ability to rapidly respond to health care emergencies by supplying a wide range of telehealth technologies and the rapidly changing way care delivery can be facilitated through the EHR and the ecosystem of apps connected to it.
Conclusion
Telemedicine helped support care delivery during the pandemic when patients were able to receive care without exposing themselves to the risk of contracting COVID-19. What’s more, telemedicine offers additional benefits of efficiency, saving both physician and patient valuable time, and expanding access to care in areas that experience provider shortages. McKinsey (2021) estimates that up to 20 percent of health spending or nearly $250 billion of health services could be provided virtually. The findings, coupled with these projections, show a need to support physicians’ telemedicine technology needs and that the technologies meet certain standards that ensure care quality and physician satisfaction.
ONC is taking a number of steps in this direction. For instance, ONC’s Cures Act Final Rule required certain developers of certified health IT to upgrade and provide, by December 31, 2022, secure, standards-based application program interfaces (APIs) using the HL7® Fast Healthcare Interoperability Resources (FHIR)® data exchange standard and make available the business and technical documentation necessary to interact with their certified API technology, and over 95 percent of those developers have done so. These requirements can enable third-party apps to connect to EHR APIs and broaden the technology available to EHR users. As these results suggest, rapid adoption of modern API technologies will likely accelerate this transformation that is already well underway.
This article was originally published on the Health IT Buzz and is syndicated here with permission.
