 By Wei Chang, Chelsea Richwine, and Samantha Meklir, ONC
By Wei Chang, Chelsea Richwine, and Samantha Meklir, ONC
X: @ONC_HealthIT
If left unaddressed, the social needs experienced by an individual may lead to poor health outcomes and more time spent in hospitals and interacting with the health care system. Hospitals, therefore, are uniquely situated to help address social needs and mitigate social risk factors by screening for social needs, assisting with transitions of care, and making connections to social service organizations. According to a recent ONC analysis of data from the 2022 American Hospital Association (AHA) Information Technology Supplement Survey, 83% of non-federal acute care hospitals collected data on patients’ health-related social needs (e.g., transportation, housing, food security), 60% received data from outside sources, and many reported using the data they collected internally and received from outside sources for various purposes. The top three uses for collected data were to inform clinical decision-making, support discharge planning, and make referrals to social service organizations. Routine data collection was less common overall (54%), and rates were even lower among lower resourced (i.e., small, rural, critical access, independent) hospitals, which has important implications for hospitals serving high-risk populations with a disproportionate share of social risk factors and social needs.
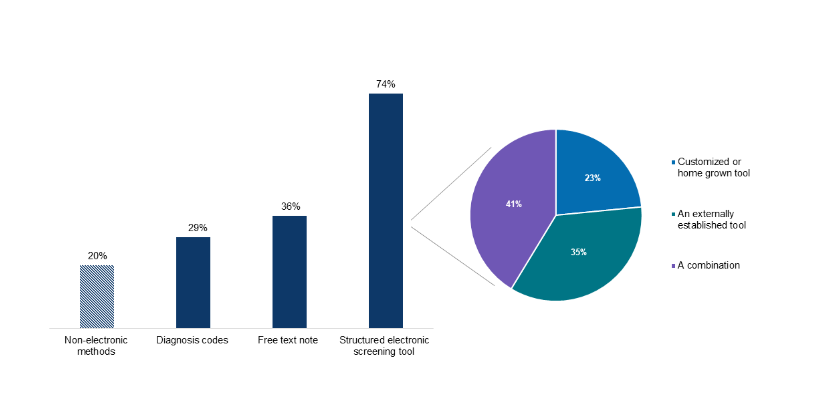
Figure 1: Methods and types of tools used to collect social needs data among hospitals that reported collecting social needs data, 2022.
How are social needs data collected?
Understanding how health care providers collect data on patients’ health-related social needs has important implications for whether and how easily those data can be shared and used. For instance, data captured in a standardized format (i.e., using a structured electronic screening tool or diagnosis codes) can facilitate data sharing with other providers for an individuals’ treatment purposes. It is more difficult to extract and exchange relevant information captured in free-text notes or non-electronic methods. Further, data captured in a standardized format where questions and responses are computable and mapped to health IT vocabulary standards (e.g., using LOINC coding terminology) helps to ensure that data captured through screening assessments are interoperable and can be shared, analyzed, and evaluated across the care continuum.
In 2022, about 3 in 4 hospitals (74%) used a structured electronic screening tool to collect social needs data and about 1 in 4 (29%) used diagnosis codes. Although we found that social needs data are largely collected in a structured format, further investigation is needed to determine the extent to which data elements in structured screening tools are mapped to existing health IT standards and coding terminology—such as those developed by the Gravity project and those referenced in USCDI SDOH data elements—to enable exchange. Similarly, keeping track of how providers are using screening tools will help identify opportunities to use validated, standardized tools that will facilitate the standardized exchange of data on patients’ health related social needs with respect to privacy regulations and protections, including applicable consent practices. For example, standardized data collection will enable the use of patients’ social needs data for care coordination and social care referrals, as well as for secondary purposes, including research and population health analytics.
Where are social needs data coming from?
While most hospitals collect internal data on patients’ health-related social needs, other health care organizations, social service organizations, and health information exchange (HIEs) organizations are critical sources of social needs data for newly admitted patients, especially in lower resourced settings that have been shown to more likely use HIEs to enable exchange. In 2022, 60% of hospitals reported receiving social needs data electronically from sources outside their hospital or health system. The most common method by which hospitals received social needs data was through HIEs (46%). In addition to data aggregation and data quality services, some HIEs, such as Maryland’s CRISP, offer more robust tools and services to assist providers in screening for and viewing patients’ past social needs data.
What’s next?
To promote routine social needs screening at hospitals, the Centers for Medicare & Medicaid Services recently added two social drivers of health measures to the Inpatient Quality Reporting (IQR) program. Social drivers of health are upstream factors that contribute to individual risk factors and differences in health-related social needs. The addition of these new measures may help ensure that a minimum set of data elements are routinely collected, which will help facilitate data exchange, while enabling hospitals to systematically collect patient level data to support whole person care.
While much attention has been devoted to screening—a critical first step to understanding patients’ health-related social needs—additional focus is needed on effective usage of data collected through screening since not all patients who screen positive for social needs are successfully connected to the resources they need. This may be attributable to a number of challenges providers face in using social needs data, including a lack of standardized referral processes and sustainable financial resources, which speaks to a need for building partnerships with community-based partners and increasing their capacity to respond at the community level, and tracking changes in health outcomes following the identification of social needs.
Looking ahead, more work is needed to capture social needs data in an actionable way so that this information can be used to support shared decision making and address social needs, with the ultimate goal of improving individual and population health.
This article was originally published on the Health IT Buzz and is syndicated here with permission.
