The following is a guest article by John Janas, MD, Medical Director at Twistle.
The COVID-19 pandemic has successfully accelerated the availability of digital health tools, while simultaneously exposing opportunity for improvement in their ability to activate patients in their care. Our nation has struggled to engage patients through patient portal apps over the past decade – indeed, while over 90% of organizations offer patient portal access, hospitals see fewer than 25% patient adoption. We have the power to reach virtually everyone in the country digitally, but we must ensure their engagement to have a real impact on the health and well-being of our nation.
As more and more healthcare interactions move online, there is a new spotlight on patient experience and seamless virtual health journeys. We’ve applied nine years of patient activation data to solve the engagement conundrum, which led to remarkable patient adoption and outcomes across a variety of COVID-19 use cases including:
- Pushing helpful information about prevention and exposure management
- Detecting symptoms of COVID-19 infection
- Remote monitoring and safe recovery from COVID-19 infection
- Collecting research data on the long-term effects of COVID-19 exposure
- Prioritizing and scheduling vaccine administration
- Managing 1st and 2nd dose reminders and adverse event monitoring
 Applying Best Practices to COVID-19-related Patient Communications
Applying Best Practices to COVID-19-related Patient Communications
We’ve analyzed patient engagement and outcome data from clients across the United States including rural and urban environments, health disparities, multiple languages, medical and surgical diagnoses, acute and chronic care episodes and more. We’ve identified a wide variety of factors that optimize patient activation in their care, which leads to greater satisfaction, better outcomes and lower costs. These basic principles were applied to our deployment of COVID-19 communications and generated equally high patient activation rates. When evaluating technologies and strategies to optimize patient engagement in their care, organizations should consider several dynamics.
 Offer Multi-modal Communication Options
Offer Multi-modal Communication Options
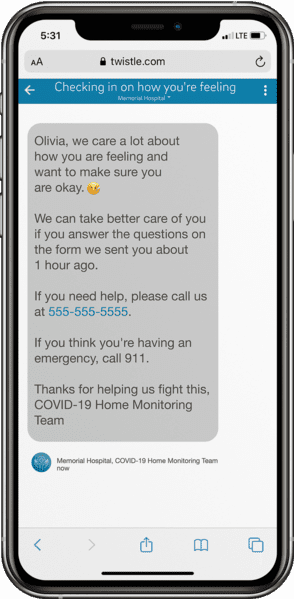
It’s important to meet patients where they live their digital lives and today — their mobile phone. Forcing patients to log in to a portal app may be a significant barrier for many people and limits the reach of your COVID-19 efforts. Conversely, according to Pew Research, 81% of Americans have a smartphone and 96% own a cell phone of some kind. Furthermore, 88% of people use their cell phone for texting on a daily basis. Healthcare organization are wise to keep communication simple by employing SMS text messages to increase engagement, while also offering other modes of communication (portal apps, third party apps, email, and even interactive voice response for those who don’t own a cell phone). By making sure patients have options to engage on their own terms, your outreach is accessible to all.
Content
Healthcare providers commonly communicate using complex medical jargon that exceeds a patient’s ability to read, understand and use the information. Messages should be short, using easy-to-understand wording and descriptive subject lines. This ensures that patients can follow instructions and respond to inquiries about their health and COVID-19 care. Provide patients with guidance in small, digestible messages that are delivered exactly when the information is needed and can be acted upon.
Message Tone
Another common practice is to build messages that only include clinical information, however, empathy has a profound impact on patient activation. Gentle nudges, friendly reminders, and encouragement help patients know that they are not alone in their COVID-19 experience. You should never underestimate the value of alleviating anxiety on the patient’s course of recovery, the patient-provider relationship, and satisfaction with their care.
Timing of Message Delivery
Asynchronous messages allow the patient to respond when it’s convenient for them, but we still find that messages delivered at certain times of the day have consistently higher engagement rates. Conversely, there are also timeframes throughout the day that are best avoided in a communication cadence because patient response rates are significantly lower.
Frequency
Patients experience message fatigue if COVID-19 check-ins occur too frequently throughout the day. Organizations must find the right balance between delivering or collecting important information and overloading patients to the point where they disengage.
Data
Ongoing analysis of patient engagement data helps organizations improve their effectiveness in COVID-19 care. Iterating on message content, timing, and so forth enables incremental improvement, which increases your reach and effectiveness in activating patients, which in turn improves clinical outcomes.
Being Responsive to Evolving Patient Care Needs
Digital communication tools, including remote and virtual technologies, moved to the forefront of care delivery in 2020 and many organizations looked to their digital health partners to quickly respond to a new reality.
Access to a flexible and configurable communication platform enables rapid response to changing patient care needs, for COVID-19 and beyond. Overcoming barriers to patient activation and positive outcomes in a fast-moving crisis can have a significant impact on patient admissions, ED visits and complication rates.
For example, Providence (Renton, WA), the first US Health System to diagnose a COVID-19 positive patient, was able to build and deploy a digital pathway that safely supported at-home recovery with remote patient monitoring within five days of project kick-off. They iterated this pathway over the first 30 days using these patient engagement best practices to further optimize care. Providence ultimately achieved 87% patient engagement throughout entire 14-day monitoring periods, safely increased nurse coordinator capacity by 400%, and realized a net promoter score (NPS) of 70, which is unheard of in healthcare!
The dynamic and evolving needs around COVID-19 vaccine coordination and administration created another challenge for health systems. Organizations that span counties and states required even greater flexibility to address eligibility requirements in accordance with local jurisdictions, prioritize them using unique criteria, notify recipients as they become eligible, obtain consent and schedule two doses of the vaccine.
Leveraging automated vaccine pathways was an effective strategy for this initial phase of vaccine administration. With a configurable digital communication platform, health systems can contact their eligible population, obtain consent, track declination, manage scheduling and deliver appointment reminders for both doses. If messaging or patient prioritization needs to be changed in response to an evolving situation, that can be completed quickly.
As the vaccine becomes available to the general public, leveraging a technology platform to provide factual and easy to understand information about efficacy, and to combat misinformation will be key in achieving herd immunity. An automated communication platform can also employ text-a-code messaging enrollment so that the public knows how to obtain the vaccine, especially in underserved communities who may not have access to a computer or a patient portal.
The Value of HIPAA-compliant Patient Communication Pathways
Healthcare IT companies have faced several unique challenges during the pandemic: an overnight shift to telemedicine, a growing list of potential symptoms to monitor, testing demands, managing the strain on facility capacities, providing routine and, in some cases, acute care remotely, and the custom requirements of each organization. This required innovation, agility, and creativity.
Twistle’s solution is accessible via text message, so engagement rates are consistently over 90%. Each pathway is carefully optimized to keep patients on track with well-timed, simple messages. This results in better adherence to care plans, improved outcomes and more satisfied patients. In addition, the platform captures data that can be used to identify opportunities for improvement, iterate existing pathways and create new pathways to support patients in their healthcare journey.

About John Janas, MD
Dr. John Janas, MD empowers Twistle clients with clinical content and best practices to manage acute and chronic conditions in the home using patient engagement and remote patient monitoring (RPM) strategies. Janas applies his 35-plus years of clinical practice experience and 25 years of EMR implementation and content development expertise to help payers, physician groups and value-based care providers improve care management and reduce costs.













