The number of hospital airborne infection isolation rooms is limited. An outbreak of infectious disease produces a demand for a large number of rooms.
The past few years navigating the COVID-19 pandemic have highlighted areas of improvement in healthcare. Healthcare facility managers have come to terms with the extreme realization of the critical importance of medical gas systems, the effects of increased demand on the hospital infrastructure, and the need for more hospital isolation rooms and negative pressure rooms.
As a result of pushing the facilities beyond their limits, additional considerations have been brought to light. Now more than ever, the need to address the management of infectious diseases is at the forefront.
The Necessity for Airborne Infection Isolation Rooms
Controlling the spread of an infectious disease is vital to maintaining a safe healthcare environment.
To prevent air leakage to or from rooms and minimize the spread of airborne infections, isolation rooms must be sealed. Isolation rooms, commonly called negative pressure rooms, are meant for single-patient occupancy and are designed to isolate airborne pathogens.
A room classifies as a negative pressure room when the air pressure inside the room is lower than the air pressure in the surrounding areas. The internal air is forced out to create negative air pressure, pulling air passively into the system from other inlets.
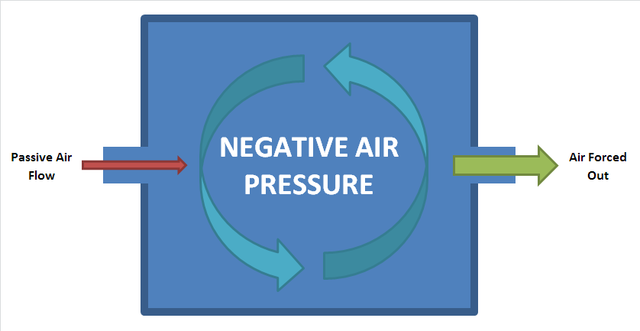
Image credit: Rrobotto, Negative Air Pressure CC BY-SA 4.0, via Wikimedia Commons
Isolation rooms are negatively pressurized with respect to adjacent areas to prevent airborne contaminants from drifting to other places and contaminating patients, staff, and sterile equipment. When a door leading to a negative pressure room opens, air from the outside area will enter. Inside air contaminated with harmful particles, should only leave through filter systems.
According to the CDC, the rooms should provide negative pressure so that air flows under the door gap into the room...
" an airflow rate of 6-12 ACH (6 ACH for existing structures, 12 ACH for new construction or renovation, and direct exhaust of air from the room to the outside of the building or recirculation of air through a HEPA filter before returning to circulation (MMWR 2003; 52 [RR-10]; MMWR 1994; 43 [RR-13]). [source]
To anticipate future outbreaks of contagious diseases, it is vital that hospital ventilation systems are in proper working order. When the pandemic first hit, we also discussed COVID-19 and negative pressure rooms in hospitals. As the pandemic appears to be coming to an end, this topic is still relevant.
Although COVID-19 was not initially considered an airborne disease, according to the CDC, a patient known to have contracted the coronavirus can spread it from person to person. This means that people in close contact with one another (within about 6 feet) can be exposed to respiratory droplets produced when an infected person coughs or sneezes.
Many facilities are choosing to place potentially infected patients in isolation rooms when resources allow.
Results of a study led by the University of Maryland School of Public Health show the evolution of the COVID-19 virus to get better at becoming airborne.
"Our research indicates that the variants just keep getting better at traveling through the air, so we must provide better ventilation," says Dr. Don Milton, professor of environmental health at the University of Maryland School of Public Health (UMD SPH).
Airborne Infectious Disease Management
The infected patient surges hospitals are experiencing reveal the need for facilities to accommodate the increased capacity.
Is your healthcare facility prepared for a surge or resurge of cases in your area?
Hospitals can start identifying areas that could be engineered as temporary negative pressure rooms to accommodate the overflow. All healthcare facilities should begin to take a new approach to solve the need for extra rooms.
Hospitals are seeing the importance of repurposing existing healthcare spaces to accommodate patient capacity. Hospitals can invest in temporary cost-effective rooms. As infection control remains a top priority, temporary containment solutions solve the problem of surges in contagious patients.
STARC, known for its reusable wall containments, is designed to hide the disruption of renovations and can also be used for effective infection control.
Watch the video below to see how a STARC reusable wall containment is used in healthcare and corporate applications.
source: STARC Systems, Overview: Reusable Temporary Wall Containment, via YouTube
The benefits of a temporary build are endless - from allowing for cost-effective options. Temporary builds are fast to install, easily and quickly disinfected, and great at segregating noise and dust.
However,
The most significant advantage is the extra space to care for your patients. Wall containments offer hospitals a solution to reduce the risk of transmission of viral infections, including COVID-19.
The air cannot escape to other sections of your facility when the door is closed, and the hospital ventilation system is operating correctly.
American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) Standard 170, Ventilation of Health Care Facilities, requires each isolation room to have a permanently installed visual device or mechanism to constantly monitor the air pressure differential of the room when occupied by a patient who requires isolation.
In Summary
Infection control remains the cornerstone for minimizing the transmission of infectious diseases. Hospitals have insufficient facilities to provide airborne infection isolation for large numbers of patients when the disease presents itself in a short amount of time.
Temporary negative pressure isolation rooms are a safe alternative for hospitals lacking the space in preexisting airborne infection isolation rooms. Facilities can use them to meet the increased surge capacity for patient isolation.
When rooms are not adequately pressurized (negative or positive), airborne contaminants can escape putting the health of patients, staff, and visitors at risk.
CHT offers medical gas services to help you reach your compliance goals and keep your hospital safe.




