In the healthcare industry, remaining compliant with federal and state regulations is of utmost importance. One vital aspect of this responsibility is that organizations monitor vendors and vendor owners to prevent payment to excluded entities or individuals. The Office of Inspector General (OIG) mandates that healthcare organizations conduct regular exclusion checks to avoid severe consequences, such as civil monetary penalties (CMP), legal ramifications, and reputational risk. Despite such mandates, OIG investigations over the past five years have found that vendors are accountable for much of the healthcare ecosystem’s fraud, waste, and abuse.
Healthcare vendors encompass a broad spectrum of entities and individuals who provide goods or services to healthcare organizations in exchange for payment. While medical providers comprise a large percentage of healthcare vendors, other facility staff members also fall under this category. This includes physicians, nurses, custodians, cafeteria staff, lawn care, and laundry personnel. A common misconception is that vendors are solely involved in patient care, but in reality, any individual or entity receiving direct or indirect payments within the healthcare sector qualifies as a vendor.
Understanding the Current and Future State of Vendor Monitoring
Vendor exclusion monitoring plays a pivotal role in upholding federal and state regulations and preventing fraudulent and abusive activities. Over the past several years, OIG has discovered that a significant amount of fraud, waste, and abuse occurs within the vendor domain. The OIG has not only required that healthcare organizations monitor their vendor populations for federal and state exclusions but also monitor vendor owners with a 5% or greater stake in the business. With approximately 18.3% of the GDP tied to the healthcare industry, it’s no wonder fraudulent individuals seeking to exploit the healthcare system often target large organizations to hide within their vast network of vendors.
But failure to effectively monitor vendors for exclusions can have severe consequences for healthcare organizations. PwC’s 2020 Global Economic Crime and Fraud Survey found that one in five (19%) organizations cite vendors and suppliers as the source of their most disruptive external fraud. In addition, alarming numbers reveal that out of the 210,000 excluded individuals in the United States, only 12,000 have an organization name attached to them. This seems to suggest that excluded individuals continue to operate within their network of influence under different names or entities.
ProviderTrust data has also shown that 20% of vendor information changes annually. Keeping track of business information, ownership details (which are not readily available to the vast majority of healthcare organizations), and other pertinent data is crucial to ensure organizations do not hire fraudulent vendors unknowingly. Capturing vendor data is complex and often not complete – for example, organizations may have the first name but not the address, etc. Failing to update this information regularly puts healthcare organizations at risk, exposing them to potential legal and financial repercussions, not to mention reputational damage.
Strategies for Effective Vendor Exclusion Monitoring
Effective vendor exclusion monitoring is crucial for healthcare organizations to maintain compliance with federal and state regulations. To ensure a robust monitoring process, organizations should adopt the following best practices:
- Comprehensive vendor coverage: Include all vendors in the monitoring process, whether they provide medical services or non-clinical goods and services. Your monitoring should cover any individual or entity receiving direct or indirect payments from the organization.
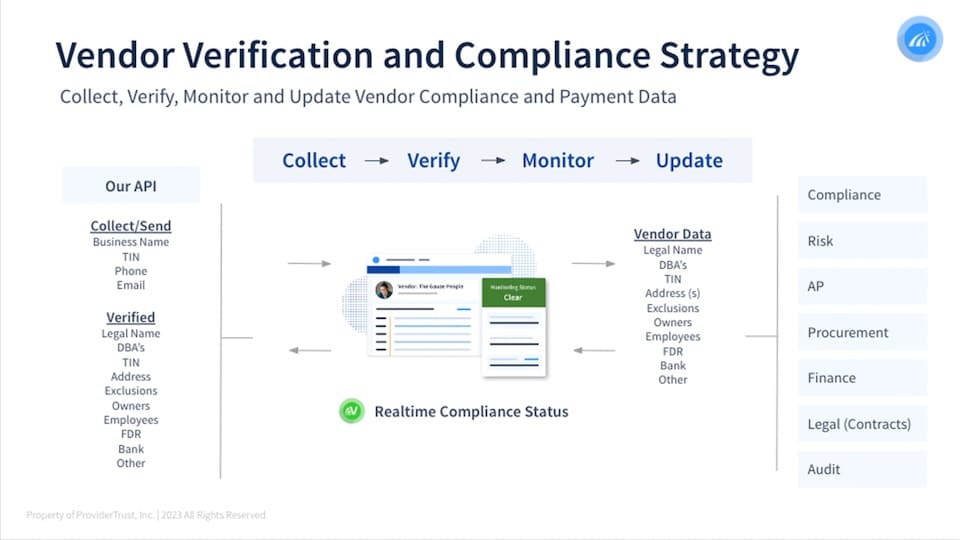
- Gather vendor information: Obtain as much information as possible from vendors to conduct exclusion checks accurately. Key details include the vendor’s business and legal name, comprehensive ownership information, tax identification number (TIN), phone number, and email address.
- Regular, automated monitoring: Conduct exclusion checks on all vendors regularly. Ideally, organizations should run checks on a monthly basis. However, real-time, automated monitoring is a great way to promptly identify any changes in vendor status as soon as they occur.
- Cross-reference exclusion lists: Integrate your monitoring system with other federal and state exclusion lists to ensure complete compliance with all regulations.
The Importance of Technology in Streamlining Vendor Monitoring
License and exclusion monitoring of vendors can be a time-consuming process that often depends on manual checks and mountains of paperwork. However, technological advancements in automated programs have revolutionized provider monitoring. With the implementation of state-of-the-art software solutions and centralized databases, healthcare organizations can now automate the process of cross-referencing vendors against state and federal exclusion lists.
One of the greatest benefits of technology-driven monitoring lies in its efficiency and accuracy. Automated systems can search through vast databases of exclusion lists in seconds, identifying vendors who have been excluded due to legal violations, fraud, or misconduct. Real-time monitoring allows healthcare organizations to proactively address compliance issues, mitigate potential risks, and prevent fraudulent activity.
Technology also streamlines license and exclusion monitoring by centralizing provider information and creating a unified platform containing vendor credentials and certification information. This ensures your organization — including compliance officers and administrators — have access to the most up-to-date vendor data as it is updated and made available.
Implications and Consequences of Non-Compliance
Failing to conduct effective vendor exclusion monitoring can have serious ramifications for healthcare organizations. The most immediate consequence is the risk of financial penalties. If healthcare organizations pay vendors who are excluded from federal healthcare programs, they may face civil monetary penalties imposed by the OIG. The average fine for an OIG exclusion ranges between $50,000 and $140,000, and this can lead to significant financial burdens that impact an organization’s resources and stability.
Another significant consequence concerns reputation Non-compliance with vendor exclusion monitoring can lead to organizations being associated with vendors who engage in fraudulent practices. This can severely affect an organization’s reputation within the healthcare industry, not to mention among patients and stakeholders. Trust and confidence in the organization’s ability to uphold ethical standards may be compromised, resulting in a loss of business and community support. Rebuilding the damaged reputation of a healthcare company is a challenging and time-consuming process that can deeply affect an organization’s long-term success.
Failing to monitor vendors for compliance can expose healthcare organizations to a wide range of legal, regulatory, and reputational consequences. Non-compliance with exclusion regulations may trigger investigations by government agencies and potential legal actions. The organization may face audits, investigations, or lawsuits, leading to additional costs and resource-intensive legal processes. To avoid these consequences, healthcare organizations must prioritize effective vendor exclusion monitoring to ensure they are fully compliant with federal and state regulations.









