It’s time for the annual ASCO conference, currently convening the American Society for Clinical Oncology in Chicago. Starting 2nd June, there have been dozens of positive announcements updating research and therapies bringing hope to the 2 million new patients who will be diagnosed with cancer in the U.S. in 2023, and millions of more people worldwide.
Just in time for #ASCO2023, the IQVIA Institute published their annual report on Global Oncology Trends 2023 – Outlook to 2027, an update featuring pipelines, therapy approvals, research updates, costs of oncology products, and patients.
I’ve pulled out three lenses on patient trends that are helpful in the context of the ASCO ’23 news, keeping the patient-as-consumer in mind. These focus on the cost of drugs at-launch; the continued challenge of diversity and inclusion in trials, access, and outcomes; and, the disruption of cancer diagnostic testing during COVID-19 which finds some patients diagnosed later and with more advanced conditions.
For many years my use of the words “health consumer” have rubbed many folks the wrong way: after all, how can patients be consumers without the requisite economic foundations that define what a “consumer” in a “health care market” are?
Points well-taken, but my perspective through my own health economics lens has been that the more costs are borne by a patient, the more that person grows (or should grow) consumer-style “muscles.” Again, it’s arguable that cancer treatment is “shoppable,” and yet people-as-payers are often compelled, based on their health insurance status and health plan design, to spend many times the median value of a U.S. family income — most recently pegged at around $70,000.
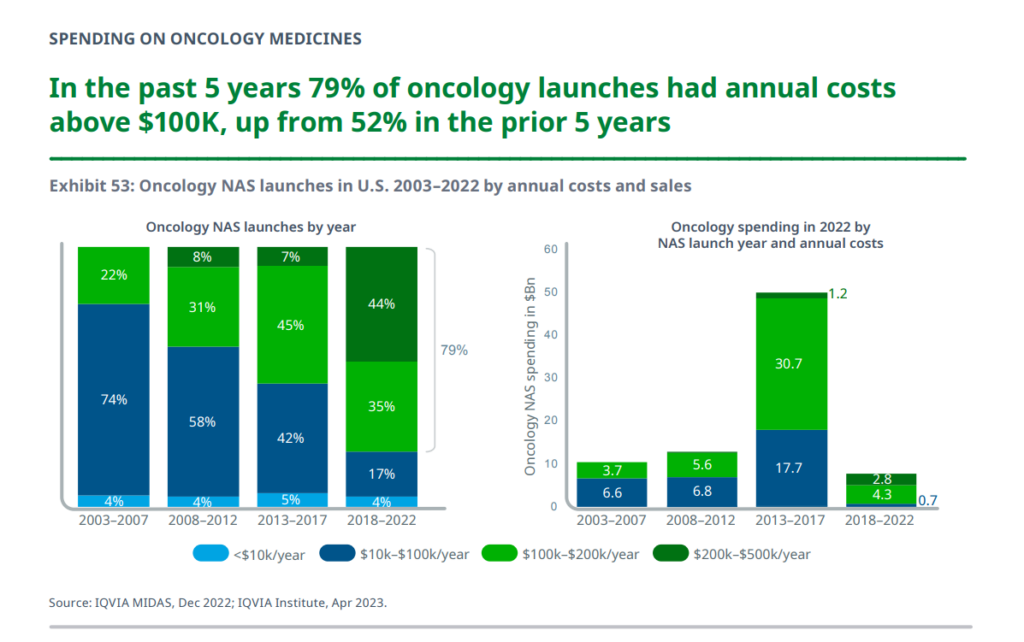
Globally, cancer medicine spending increased by 4% to nearly $200bn, underpinned by new therapies coming to market and expanding access.
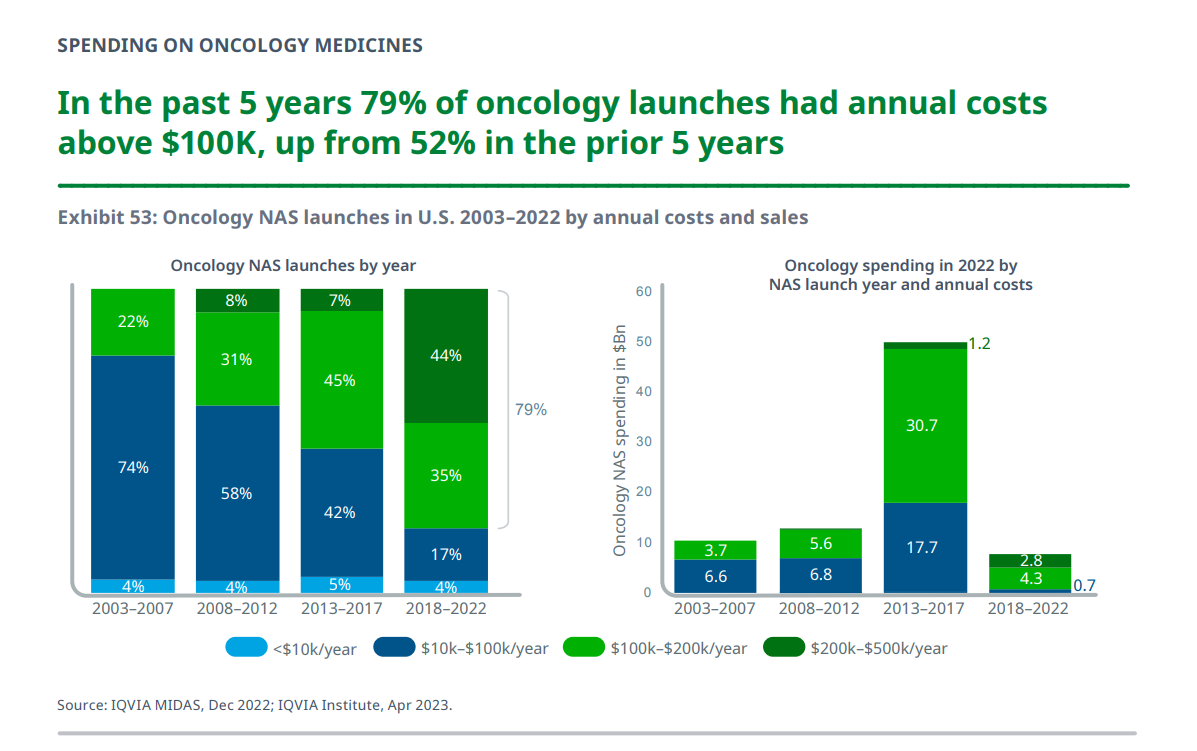
With a focus on the U.S., the number of new cancer drugs used in the U.S. health system had costs over $200,000 a year, making up 44% of launches in the past five years, shown in the bar chart from the report.
New cancer drugs with costs over $100,000 comprised 79% of launches in the past five years, from 52% over the previous five years.
Note that “cost” here does not equate to what patients eventually pay out-of-pocket for the therapy: IQVIA Institute notes that, “While individual drugs can have a high cost, the cost of a patient’s treatment continues to vary based on the overall regimens they receive and non-drug components of their care, and can especially be influenced by their insurance type.” 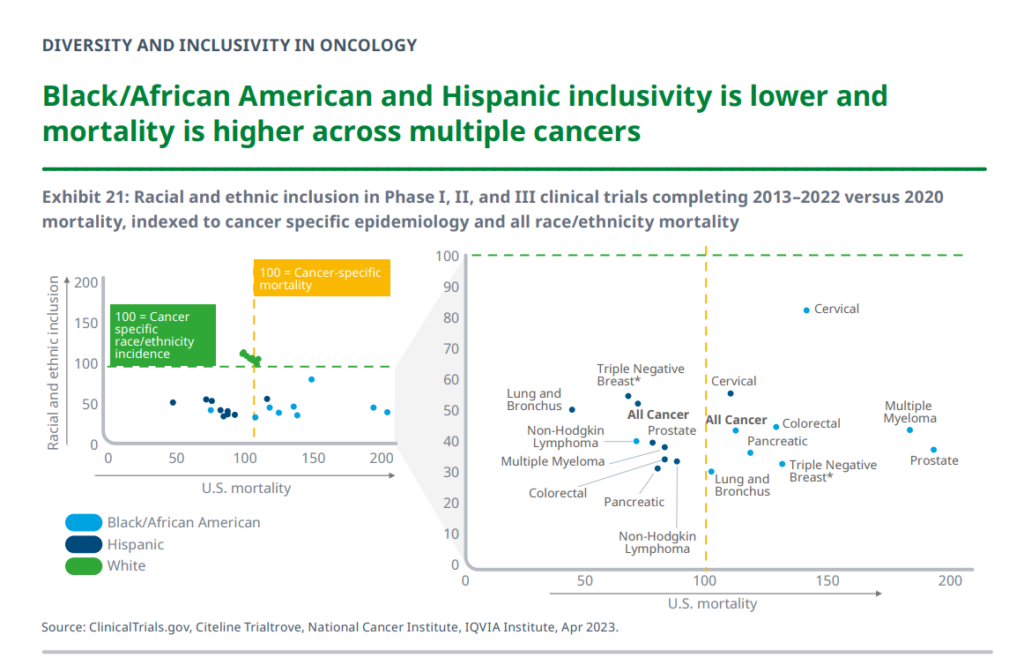
The second point I’ll pull out of this report comes from a section of important data on diversity and inclusivity in oncology. There are several insightful observations to share, with this one incorporating two key points:
- The inclusion of Black/African American and Hispanic patients in clinical trials completed between 2013-2022 was lower than that for whites, proportionately; and,
- Mortality rates for Black/African American and Hispanic patients is higher across many forms of cancer.
As the report calls out, simply put, “In all analyzed cancers but non-Hodgkin lymphoma, Black/African American patients experience higher than the U.S. mortality rate. In the cases of multiple myeloma and prostate cancer, Black/African American patients experience mortality at nearly twice the cross-population rate at 84% and 92%, respectively, above cancer-specific U.S. mortality rates.”
More generally, IQVIA’s analysis shows that disparities exist across demographic groups in both socioeconomic status and cancer outcomes, with 12%
higher mortality in Black/African American populations than other demographic groups, they report.
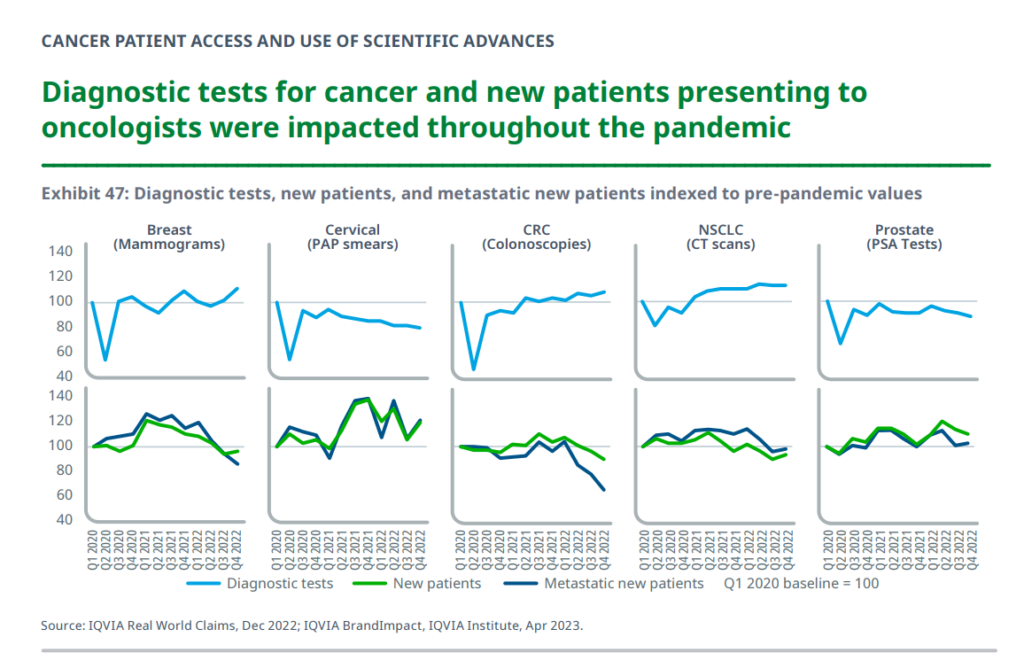
Next, to diagnostic testing for various cancers which was dramatically disrupted by the coronavirus pandemic. See the “v’s” shown in each graph here, tracking testing declines for five cancer types: breast (mammograms), cervical (PAP smears), CRC (colorectal cancer, colonoscopies), NSCLC (lung cancer, CT scans), and prostate (PSA tests).
While mammogram screenings have largely recovered to previous levels, IQVIA data shows, more women have been newly diagnosed and more have been metastatic at the diagnosis, implying that the early impact (drop) in diagnostic testing may have caused later diagnosis for some of the patients.
Cervical cancer screenings fell over the past few years, with numbers for new and metastatic patients higher. In addition, colonoscopies have returned to baseline, IQVIA observes, with more home testing which is not captured in these data.
Health Populi’s Hot Points: Consider these Three summary points presented in IQVIA’s report overview which capture my 3 curated slides’ points:
- “The costs associated with treating more patients for longer and with more advanced therapies is bringing stress to healthcare budgets, even as the broader adoption of biosimilars provides some relief.”
- “Despite significant advances in treatment, the global oncology community and patients continue to struggle with disparities in access and care.”
- “Novel treatments have improved patient outcomes across a range of cancers, but differences in access may lead to variability in care.”
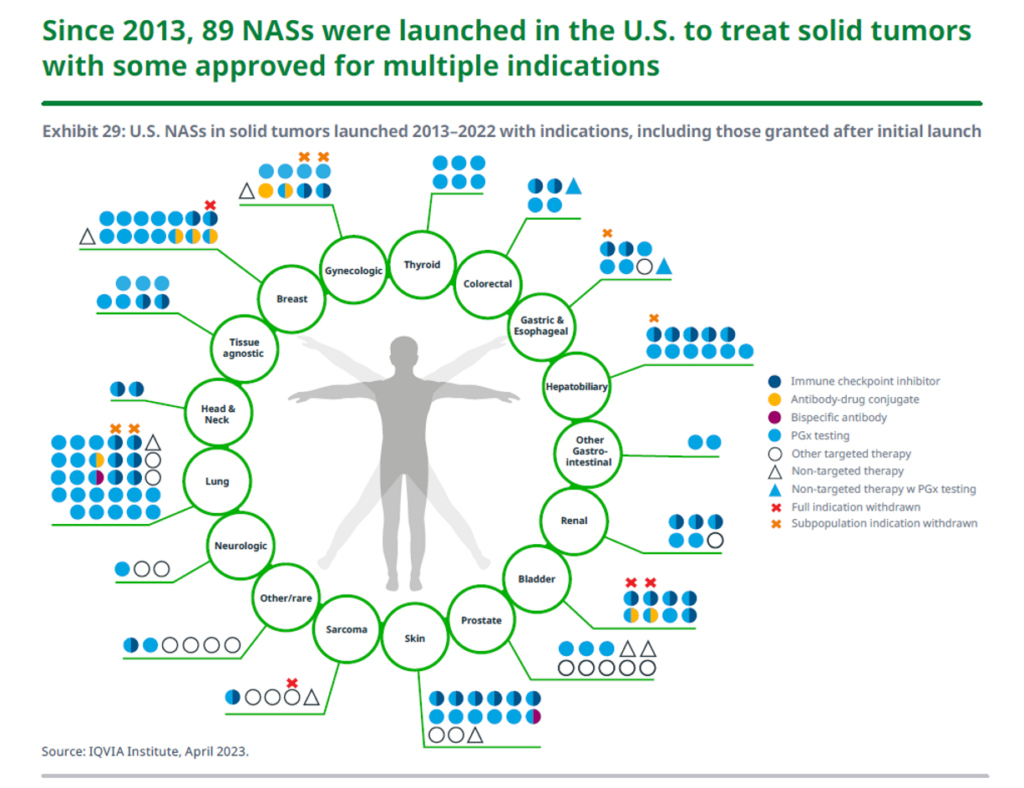
With a “surge” of oncology R&D, demonstrated by ASCO 2023 reports and press releases. This chart from the IQVIA report tells part of the innovation story, for new oncologic drugs for solid tumors — as you can see by the aggregation of dots, lung cancer tx launches have been particularly productive, along with breast cancer, along with a number of new therapies for skin cancers (melanoma).
With these new product launches come the discussion about “who pays” for innovation, globally: the U.S. (including patients living in the U.S.) have long borne marginally higher costs for access to these therapies.
In 2023, kudos go to ASCO for putting the role of patients front and center in the meeting. A key theme for #ASCO2023 is “Partnering with Patients,” which will be featured in various sessions and clinical findings. Relevant to the challenge of health equity and disparities will be research demonstrating that Medicaid expansion led to lower mortality and racial disparities for gastrointestinal cancer, compared with patients residing in states which did not expand Medicaid.
Given the growing population of more activist patients, such as those participating at ASCO like my collegial friends Grace Cordovano and Stacy Hurt, among many others, we can see new models emerging for oncology drug/therapy pricing and cost-management. One area to watch is the “Mark Cuban Effect,” discussed in this post by two oncology clinicians who explain how the Cost-Plus model shows promise for some patients and some types of therapies. This is not a panacea to solve the over-arching challenge of who pays for and invests in innovation for cancer, but more transparency and creativity is clearly emerging with the promise of patients partnering with industry for access, inclusion, equity, and ultimately, better outcomes for all.

To that end, exciting news was announced this weekend during ASCO 2023 on the formation of CancerX, a community of stakeholders committed to crushing cancer – across the ecosystem, from patients to providers, life science companies and researchers to med-tech innovators, technology platform players and digital health developers.
The map covers the many founding members of CancerX, inspired and motivated by the White House Cancer Moonshot announced in February 2023 — to end cancer as we know it.
Onward….




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.