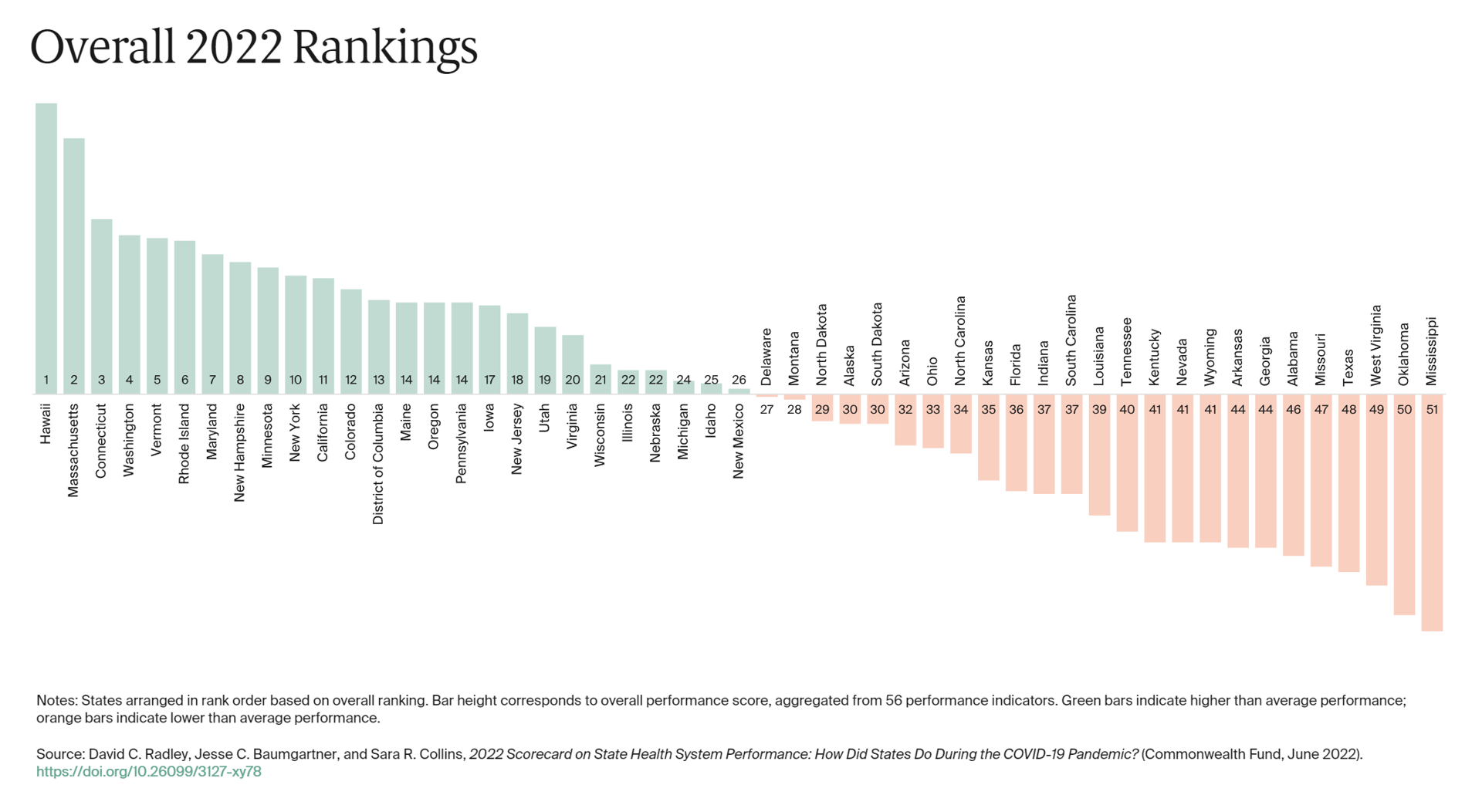
The best U.S. states to live in for health and health care are Hawaii, Massachusetts, Connecticut, Washington, Vermont, Rhode Island, and Maryland…
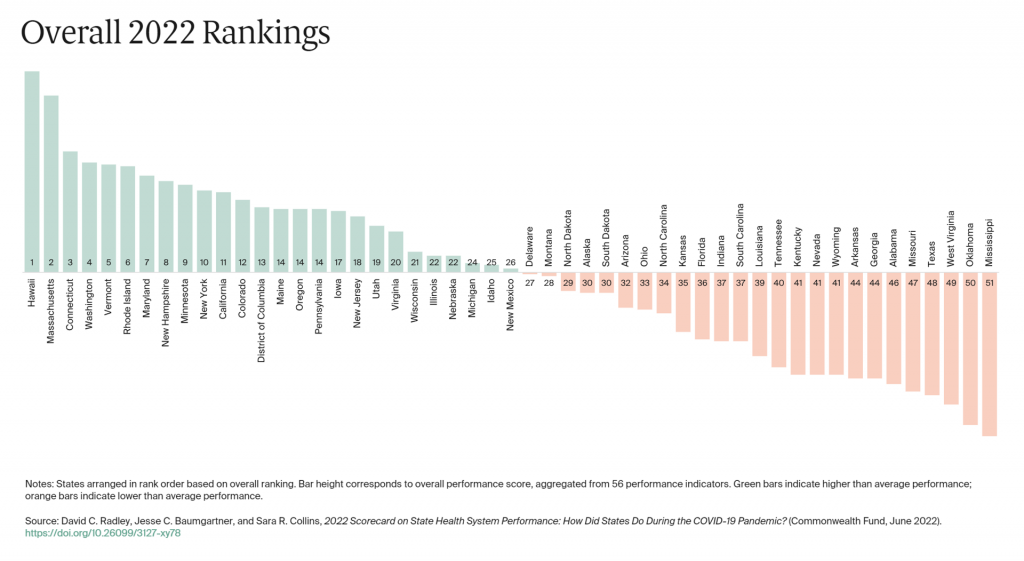
Those are the top health system rankings in the new 2022 Scorecard on State Health System Performance annual report from the Commonwealth Fund.
If you live in Mississippi, Oklahoma, West Virginia, Texas, Missouri, Alabama, Georgia, or Arkansas, your health care and outcomes are less likely to be top-notch, the Fund’s research concluded.
The Commonwealth Fund has conducted this study since 2006, assessing a range of health system indicators and patient outcomes to track trends over time identifying which U.S. states set the bar higher for their health citizens’ well-being.
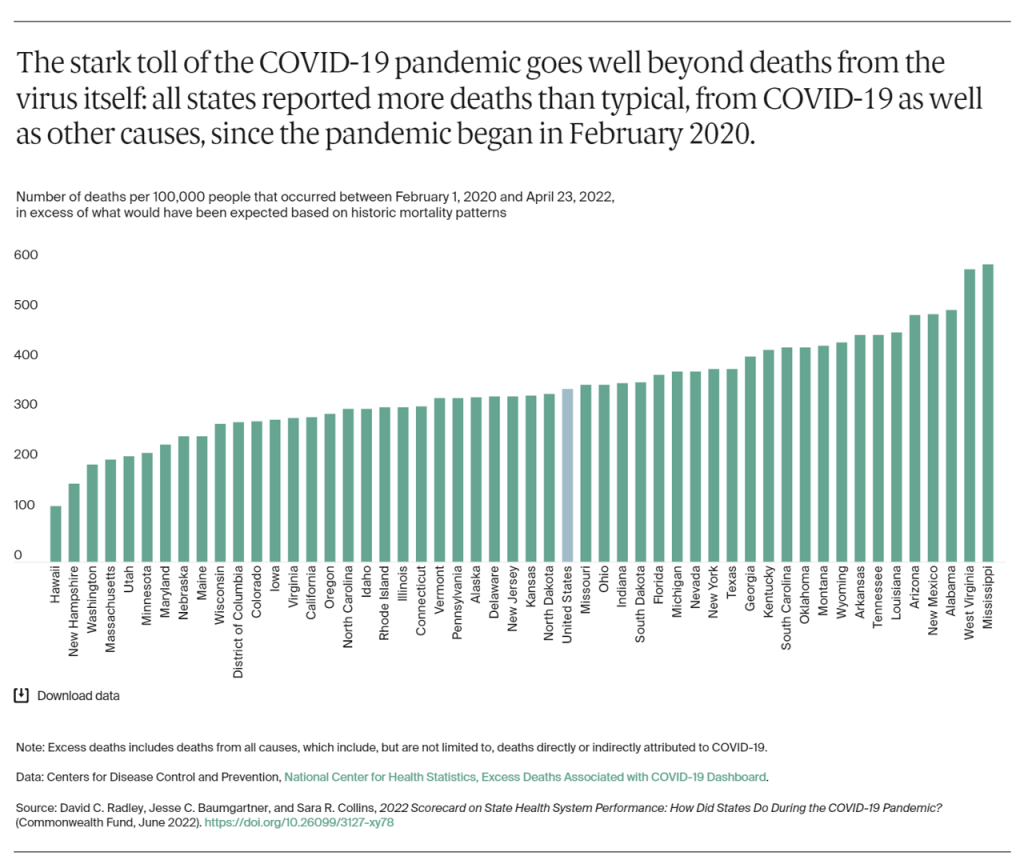
In previous years, of course, the coronavirus had not played a role in quantifying certain aspects of health system performance. Here for 2022, the second chart tracks the “stark toll” of the COVID-19 pandemic and the excess deaths experienced for each state since the pandemic emerged in February 2020.
With respect to the pandemic, we see a similar pattern in state rankings here, with the top ten performers generally consistent with those in the overall rankings. Ditto for the bottom rankings, with Mississippi and West Virginia ranking 50th and 49th in the number of deaths per 100,000 people that occurred between February 1 2020 and April 23 2022, in excess of what would have been expected based on historic mortality patterns.
[For more details on the concept of “excess deaths,” see this post in Health Populi with the details].
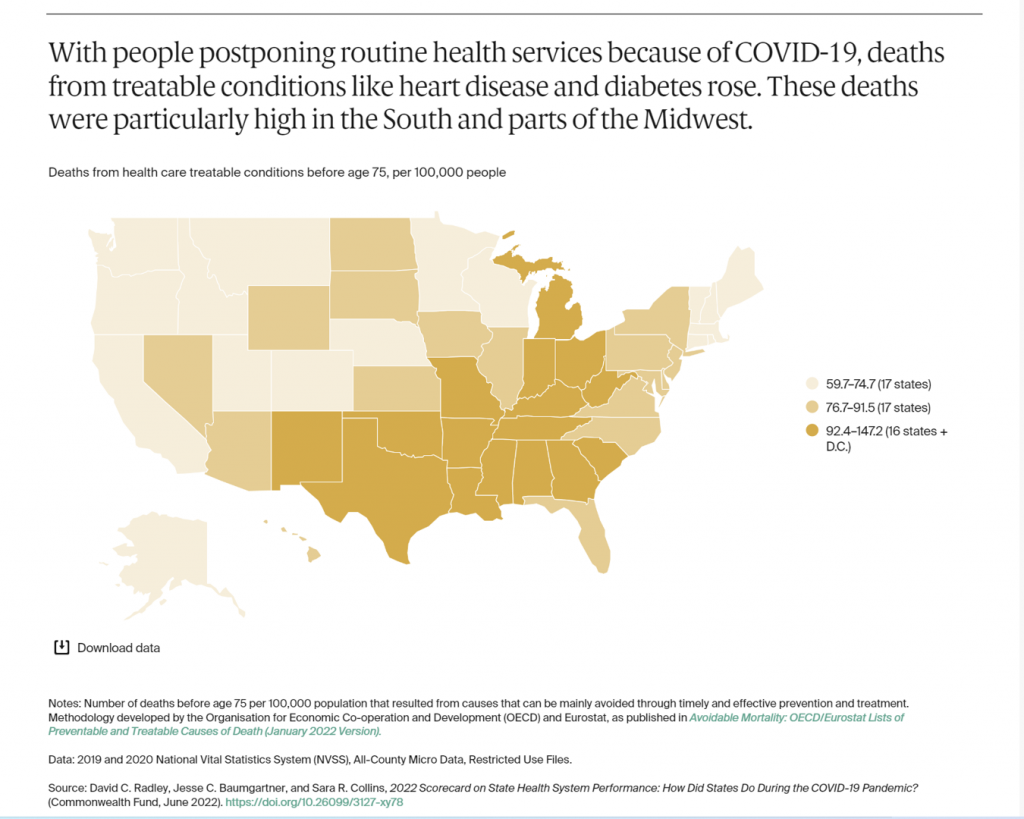
This map illustrates death rates per 100,000 people from treatable conditions impacting folks before age 75. Note the darker shaded states in the Southern U.S. and some Midwestern states.
These conditions, such as diabetes and heart disease, exacerbated for some patients due to peoples’ “medical distancing” — avoiding or postponing outpatient visits for routine health services and chronic care management.
The overall death rates for this scenario increased from 83.8 to 89.8 deaths per 100,000 population between 2019 and 2020.
Pre-pandemic, that rate was even for eight years, then this jump spiked in 2020.
Health Populi’s Hot Points: Your ZIP code can shape your health more than your genetic code: you have heard this public health mantra by now, thanks to the pioneering work of Dr. Tony Iton who figured out the role of local factors beyond medical care on the well-being of Alameda County, California, health citizens, following his early years in medicine working in Baltimore.
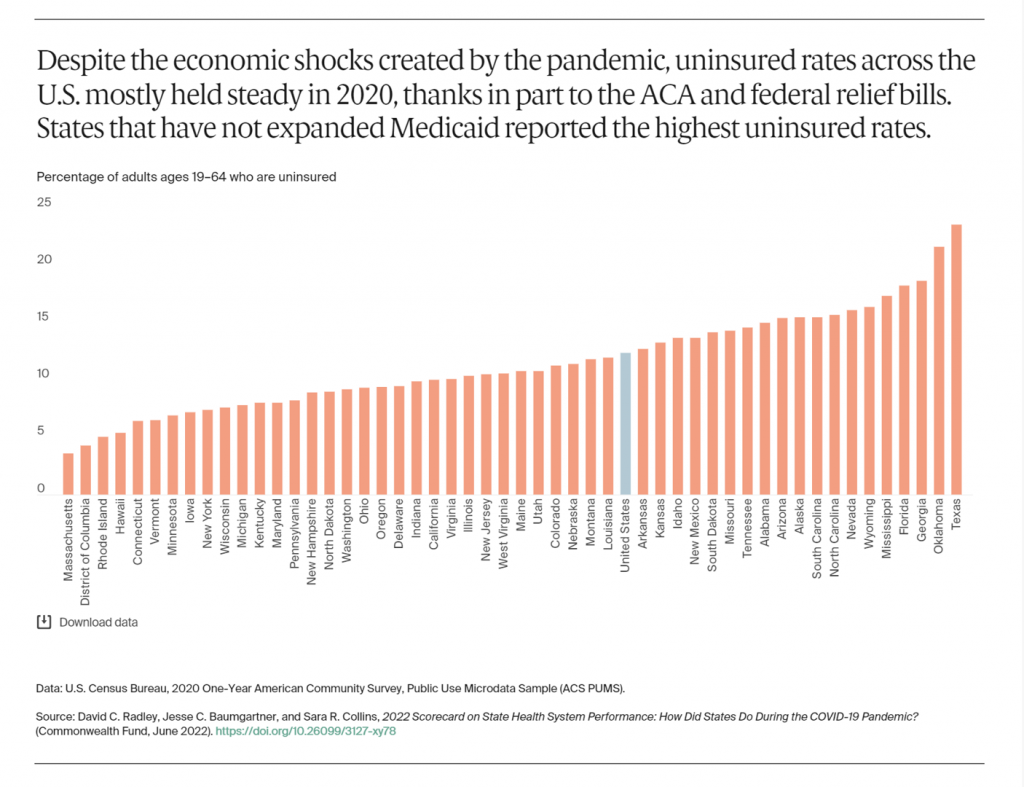
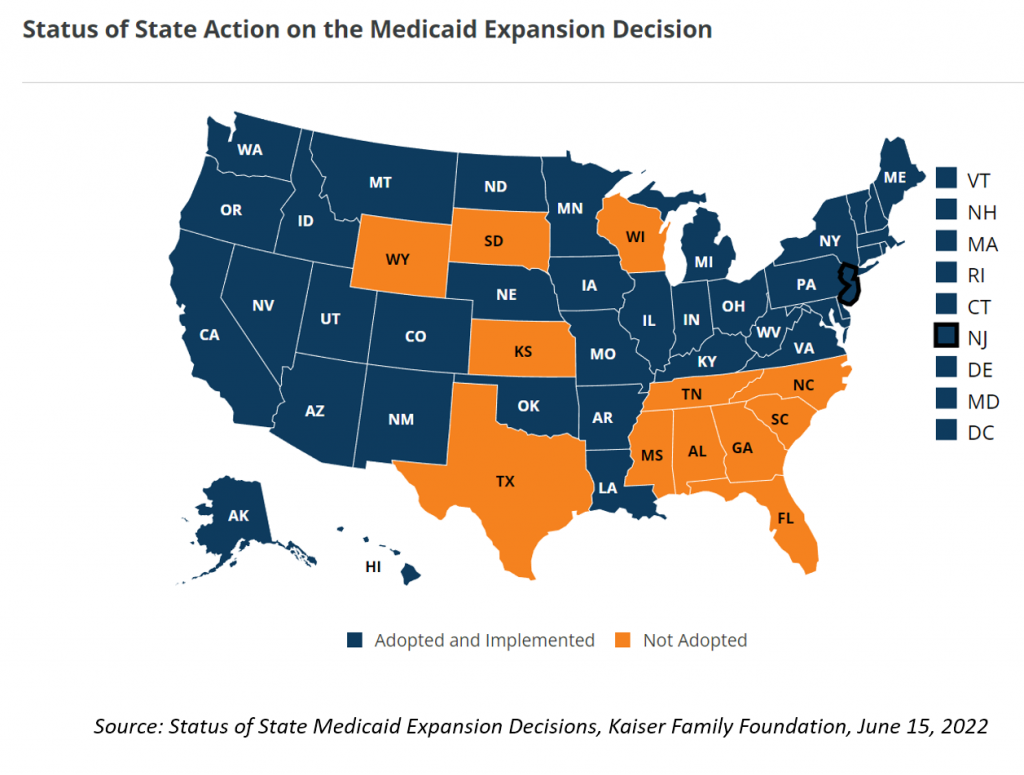
The last chart from the Commonwealth Fund 2022 State Scorecard talks about the rate of uninsurance by state — think ZIP code or personal GPS — calling out the fact that a dozen Governors did not expand Medicaid to accommodate ACA health plan enrollment for their health citizens.
I’m sympathetic to the fact that U.S. State Governors’ top line items in budgets are education and health care. But ironically, these spends go hand-in-hand, because education is, arguably, the most important determinant of health. Investments in public education, especially in early childhood and then ongoing for building up children’s, adolescents’, and teen’s human capital, bolsters health and well-being over those kids’ lifetimes.
At the same time, check out the map here and other maps in the full report on the Commonwealth Fund’s website. You’ll spot the trend, that people living in certain states have had poorer health outcomes as well as less productive health system performance.
Connect the dots between the drug overdose deaths (chart above), excess deaths (noted in the second chart, above), and states with fuller ICUs over extended periods of time, among other indicators. Those states also tend to have greater risks of people living with obesity, diabetes, and other chronic conditions, along with greater rates of smoking that exacerbate risks of many chronic disease and mortality.
The Fund’s bottom line. learned over many years of curating this Scorecard study: “States that have historically performed well on our State Scorecard also performance well as the pandemic unfolded, based on our usual set of health system measures and the new COVID-19-specific measures.” Furthermore, states should boost investment in primary care – “the foundation for a high-performing health care system” — and fully integrate behavioral and mental health services with primary care.
Finally, invest “broadly” in social services to address factors that are determinants of health and well-being, like housing and economic security.
The final call-to-action: states should strengthen insurance coverage and care delivery systems to better withstand future health emergencies.
Because these public health emergencies will continue to live with us, in every ZIP code.




 I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful.
I'm in amazing company here with other #digitalhealth innovators, thinkers and doers. Thank you to Cristian Cortez Fernandez and Zallud for this recognition; I'm grateful. Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.